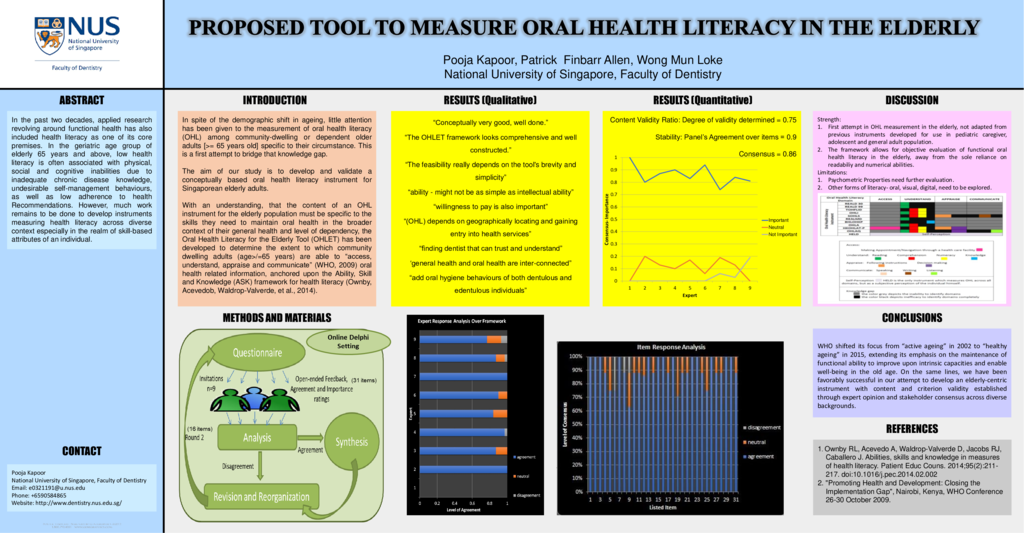
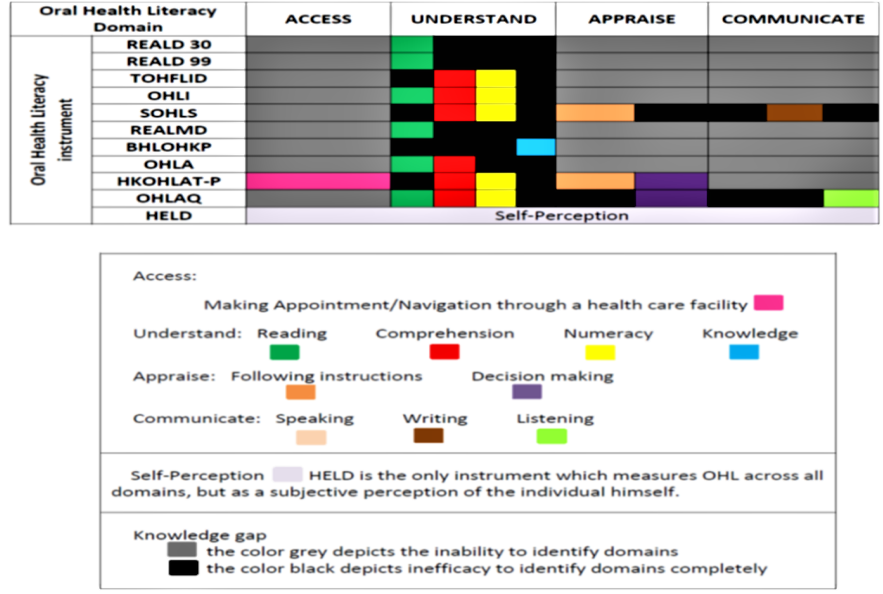
Background: The world’s adult population of 65 years and above, commonly referred to as the “elderly” is rapidly increasing and so are their oral health needs. In the past two decades, applied research revolving around functional health in this population has also included health literacy as one of its core premises. In the geriatric age group, low health literacy is often associated with physical, social and cognitive inabilities due to inadequate chronic disease knowledge, undesirable self-management behaviors, as well as low adherence to health recommendations. The continuous interaction between health literacy and determinants of health as well as health outcomes has been effectively established. However, much work remains to be done to develop instruments measuring oral health literacy across diverse contexts especially in the realm of skill-based attributes of an individual (Figure below). Aim: The current study is designed to develop and test an Oral Health Literacy (OHL) instrument for use in the multiracial multilinguistic Singaporean elderly (65+ years of age) as an initial step to assess the skill-based attributes of individuals relevant in making health related choices. Methods: Delphi method used to reach consensus on the core dimensions (e.g. Access, Understand, Appraise, Apply) targeted in the development of the OHLET (Oral Health Literacy Tool for the elderly) and to establish suitability of the items used to measure oral health literacy within each dimension (ability, skills, knowledge) with respect to the target population, including elderly across varying states of dependency and frailty. Results: Iterative Analysis: Qualitative analysis helped revise the initial instrument. Favorable Consensus generated. Content Validity Ratio: 0.75; Stability: 0.9; Consensus: 0..86. Conclusions: The global aim of the exercise has been to achieve consensus on the initial item pool relevant to the measurement of oral health literacy in the elderly. It is necessary to address oral health literacy among the geriatric age group to not only improve their health states but also to equip them to make positive behaviour change, improve knowledge base, and empower them to sustain their ability to make suitable decisions in the present as well as the future to come. Inclusion of measures of oral and digital literacy has also been explored.
- 62 views