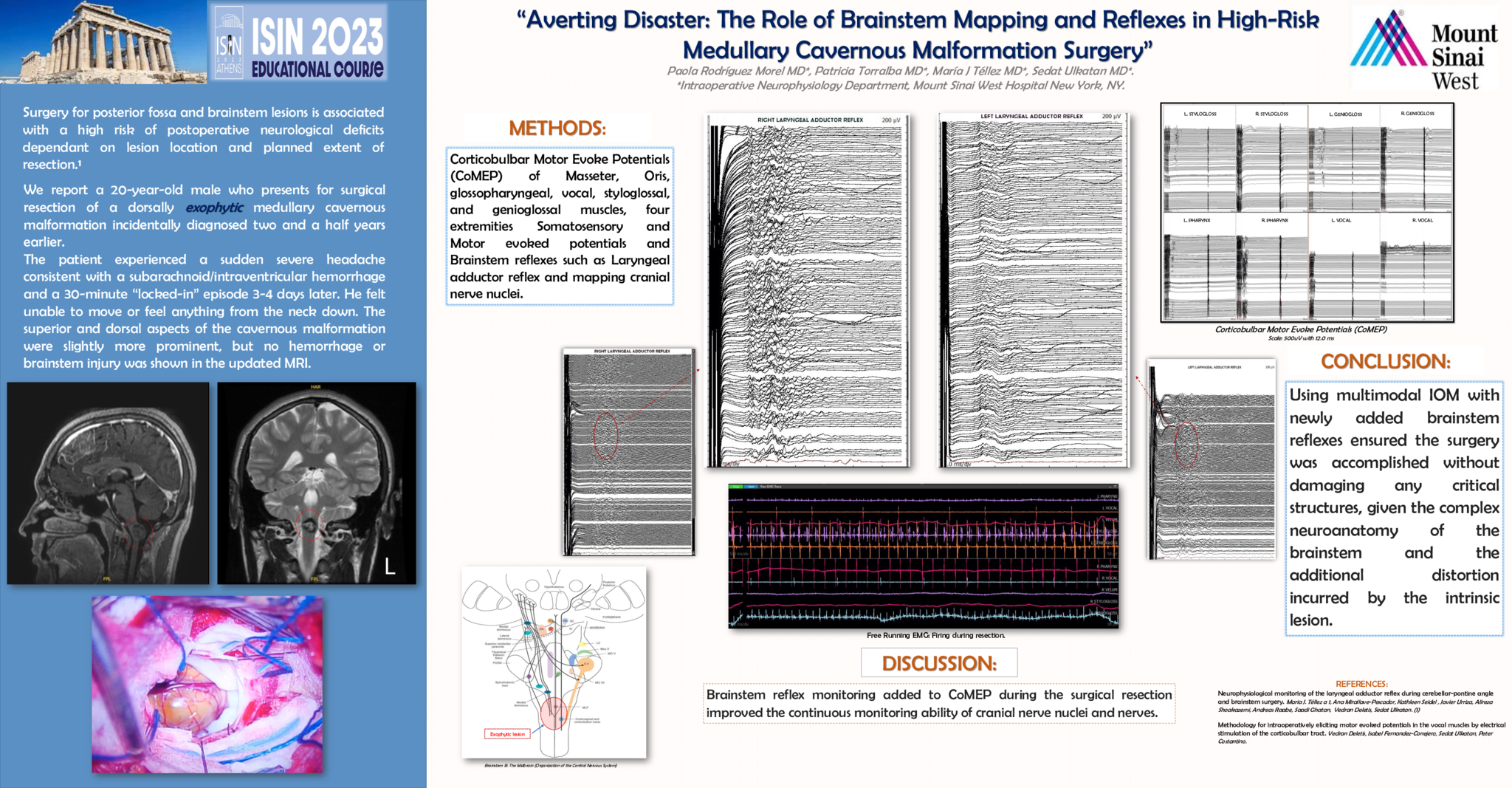
We report a 20-year-old male who presents for surgical resection of a dorsally exophytic medullary cavernous malformation incidentally diagnosed two and a half years earlier. The patient experienced a sudden severe headache consistent with a subarachnoid/intraventricular hemorrhage and a 30-minute “locked-in” episode 3-4 days later. He felt unable to move or feel anything from the neck down. The superior and dorsal aspects of the cavernous malformation were slightly more prominent, but no hemorrhage or brainstem injury was shown in the updated MRI. Methods of choice for multimodal Intraoperative monitoring were: Corticobulbar Motor Evoke Potentials (CoMEP) of Masseter, Oris, Glossopharyngeal, Vocal, Styloglossal, and Genioglossal muscles, four extremities Somatosensory and Motor evoked potentials and Brainstem reflexes such as Laryngeal adductor reflex (LAR) and mapping cranial nerve nuclei. Brainstem mapping became critical for guiding the surgeon on the less unsafe entry point for the vascular malformation approach. Brainstem reflex monitoring added to CoMEP during the surgical resection improved the continuous monitoring ability of cranial nerve nuclei and nerves. Conclusion: Using multimodal IOM with newly added brainstem reflexes ensured the surgery was accomplished without damaging any critical structures, given the complex neuroanatomy of the brainstem and the additional distortion incurred by the intrinsic lesion.
- 2 views