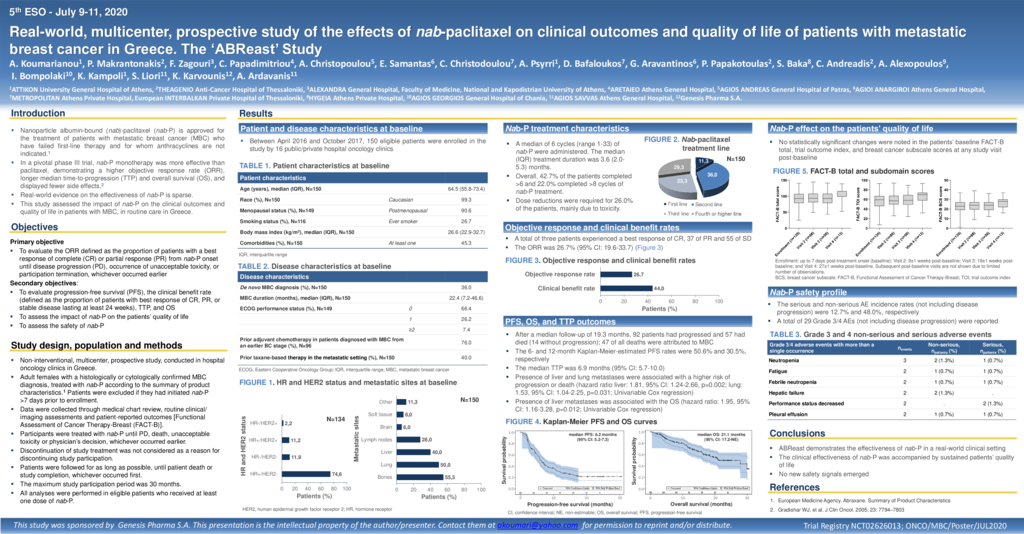
Introduction:Nanoparticle albumin-bound (nab)-paclitaxel (nab-P) is approved for the treatment ofpatients with metastatic breast cancer (MBC)who have failed first-line treatment for metastatic disease and for whom standard, anthracycline containing therapy is not indicated. Real-world evidence on the effectivenessof nab-P is sparse. From this perspective, this non-interventional study was designedto assess the impact of nab-Pon the clinical outcomes and the quality of life of patients with MBC in the routine care of Greece. Materials and methods: This multicenter prospective studyenrolledconsented females with MBC initiated (≤7 days prior to enrollment) onnab-Paccording to physicians decision. Clinicopathologic parametersand patient-reported outcomes[Functional Assessment of Cancer Therapy-Breast (FACT-B)] were collected at approximately 9-week intervals during the first 12 months of study participation and approximately every 18 weeks thereafter, until the end of the study observation period (maximum 30 months). Results:Between April 2016 and October 2017, 150eligible patients(99.3% Caucasian) were enrolled in the study in16 oncology centers.The patients’median age was64.5 years (range: 30.7-84.0) andECOG performance status was 0in 66.4% and 1 in 26.2%. 45.3% of patients had ≥1comorbidity (21.3% cardiovascular diseases). The median time elapsed since MBC diagnosis was 22.4 months, while36.0% of patients were de novometastatic. The distribution of hormone receptor (HR)/human epidermal growth factor receptor 2 (HER2) status was74.6% HR+/HER2-,11.9% HR-/HER2-, 11.2% HR+/HER2+, and2.2% HR-/HER2+. Most commonly occurring metastatic sites were the bones (55.3%), lung (50.0%), and liver (40.0%). Prior taxane-based therapy was annotated in 40.0% of patients. Of the patients, 11.3% received nab-P as first, 36.0% as second, 23.3% as third, and 29.3% as fourth or further treatment line. A median of 6 cycles (range: 1-33) were administered; 42.7% of the patients completed >6 and 22.0%>8 cycles. Dose reductions were required for 26.0% of the patients, mainly due to toxicity. The objective response rate was 26.7% and the clinical benefit rate was 44.0%. After a median follow-up of 19.3 months, 92patients had progressed and 57 had died (14 without progression). The median progression-free survival (PFS) was 6.2 months [95% confidence interval (CI): 5.2-7.3]. The 6- and 12-month PFS rates were 50.6% and 30.5%, respectively.The median overall survival was 21.1 months (95% CI: 17.2-not estimable).Liver [hazard ratio (HR): 1.81; 95% CI: 1.24-2.66] and lung (HR: 1.53; 95% CI: 1.04-2.25) metastases were associated with a higher risk of progression or death.No statistically significant change in the patients’ baseline FACT-B total score (median: 93.0) was observed. The serious and non-serious adverse event (AE) incidence rates were12.7% and 48.0%, respectively with a total of 37grade≥3AEs(not including disease progression) reported. Conclusion:This study generated real-world evidence on the effectiveness of nab–paclitaxel; no new safety signals emerged.
- 118 προβολές