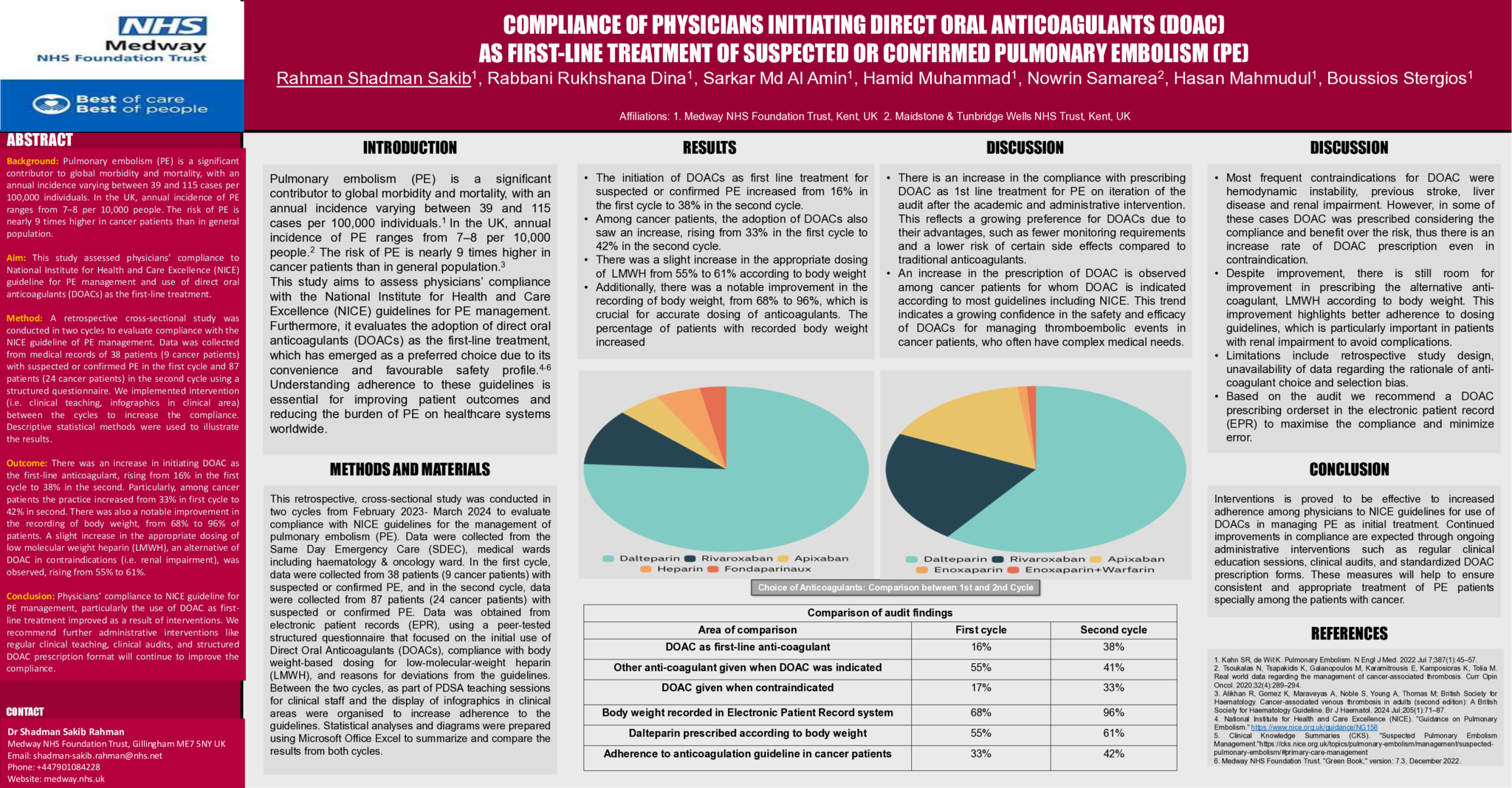
Abstract Background: Pulmonary embolism (PE) is a significant contributor to global morbidity and mortality, with an annual incidence varying between 39 and 115 cases per 100,000 individuals1. In the UK, annual incidence of PE ranges from 7–8 per 10,000 people2. The risk of PE is nearly 9 times higher in cancer patients than in general population3. Aim: This study assessed physicians’ compliance to National Institute for Health and Care Excellence (NICE) guideline for PE management and use of direct oral anticoagulants (DOACs) as the first-line treatment4-6. Method: A retrospective cross-sectional study was conducted in two cycles to evaluate compliance with the NICE guideline of PE management. Data was collected from medical records of 38 patients (9 cancer patients) with suspected or confirmed PE in the first cycle and 87 patients (24 cancer patients) in the second cycle using a structured questionnaire. We implemented intervention (i.e. clinical teaching, infographics in clinical area) between the cycles to increase the compliance. Descriptive statistical methods were used to illustrate the results. Outcome: There was an increase in initiating DOAC as the first-line anticoagulant, rising from 16% in the first cycle to 38% in the second. Particularly, among cancer patients the practice increased from 33% in first cycle to 42% in second. There was also a notable improvement in the recording of body weight, from 68% to 96% of patients. A slight increase in the appropriate dosing of low molecular weight heparin (LMWH), an alternative of DOAC in contraindications (i.e. renal impairment), was observed, rising from 55% to 61%. Conclusion: Physicians’ compliance to NICE guideline for PE management, particularly the use of DOAC as first-line treatment improved as a result of interventions. We recommend further administrative interventions like regular clinical teaching, clinical audits, and structured DOAC prescription format will continue to improve the compliance. Comparison of audit findings Area of comparison First cycle Second cycle DOAC as first-line anti-coagulant 16% 38% Other anti-coagulant given when DOAC was indicated 55% 41% DOAC given when contraindicated 17% 33% Body weight recorded in Electronic Patient Record system 68% 96% Dalteparin prescribed according to body weight 55% 61% Adherence to anticoagulation guideline in cancer patients 33% 42% References Kahn SR, de Wit K. Pulmonary Embolism. N Engl J Med. 2022 Jul 7;387(1):45–57. Tsoukalas N, Tsapakidis K, Galanopoulos M, Karamitrousis E, Kamposioras K, Tolia M. Real world data regarding the management of cancer-associated thrombosis. Curr Opin Oncol. 2020;32(4):289–294. Alikhan R, Gomez K, Maraveyas A, Noble S, Young A, Thomas M; British Society for Haematology. Cancer-associated venous thrombosis in adults (second edition): A British Society for Haematology Guideline. Br J Haematol. 2024 Jul;205(1):71–87. National Institute for Health and Care Excellence (NICE). "Guidance on Pulmonary Embolism." https://www.nice.org.uk/guidance/NG158">https://www.nice.org.uk/guidanc…; Clinical Knowledge Summaries (CKS). "Suspected Pulmonary Embolism Management."https://cks.nice.org.uk/topics/pulmonary-embolism/management/suspected-…; Medway NHS Foundation Trust. "Green Book," version: 7.3, December 2022.
- 27 προβολές