Introduction: Post-operative infections in the setting of internal fixation of tibial plateau fractures present a devastating complication and remain a huge challenge. The orthoplastic approach is essential for the management of such entities. Ιt enables to address both the soft tissues and the fracture.
Objectives: This study presents the results of patients treated with orthoplastic principles for early post-operative infection after osteosynthesis of tibial plateau fractures.
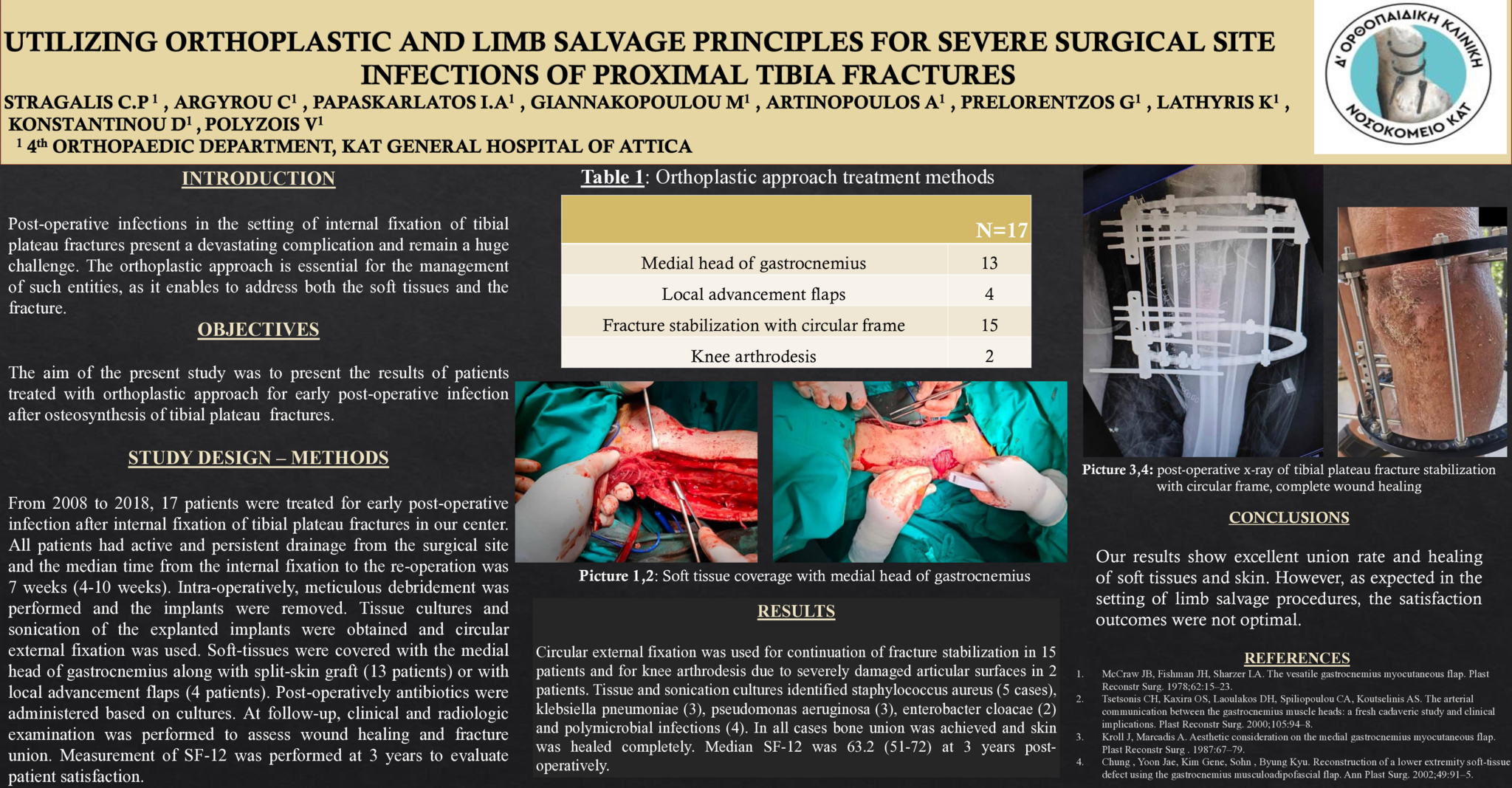
Study Design & Methods: From 2008 to 2018, 17 patients were treated for early post-operative infection after internal fixation of tibial plateau fractures in our center. All patients had active and persistent drainage from the surgical site and the median time from the internal fixation to the re-operation was 7 weeks (4-10 weeks). Intra-operatively, meticulous debridement was performed and the implants were removed. Tissue cultures and sonication of the explanted implants were obtained, and circular external-fixation was used. Soft-tissues were covered with the medial head of gastrocnemius along with split-skin graft (13 patients) or with local advancement flaps (4 patients). Post-operatively antibiotics were administered based on cultures. At follow-up, clinical and radiologic examination was performed to assess wound healing and fracture union. Measurement of SF-12 was performed at 3 years to evaluate patient satisfaction.
Results: Circular external fixation was used for continuation of fracture stabilization in 15 patients and for knee arthrodesis due to severely damaged articular surfaces in 2 patients. Tissue and sonication cultures identified staphylococcus aureus (5 cases), klebsiella pneumoniae (3), pseudomonas aeruginosa (3), enterobacter cloacae (2) and polymicrobial infections (4). In all cases bone union was achieved and skin was healed completely. Median SF-12 was 63.2 (51-72) at 3 years post-operatively.
Conclusions: Our results show excellent union rate and healing of soft tissues and skin. However, as expected in the setting of limb salvage procedures, the satisfaction outcomes were not optimal.
- 2 προβολές