Introduction/Purpose
Hallucal sesamoid traumatic dislocation represents a rare entity in the annals of orthopaedic foot trauma. Isolated traumatic dislocation of fibular sesamoid is even more uncommon and usually misdiagnosed. Only a few publications limited to case reports exist hitherto in the literature. Herein we report the case of a male adolescent with traumatic proximal dislocation of the fibular sesamoid, managed successfully with open reduction and repair of ruptured first metatarsophalangeal (MTP) joint capsule. At three months follow up, the patient was asyptomatic and had fully returned to his everyday activities.
Method/Case study
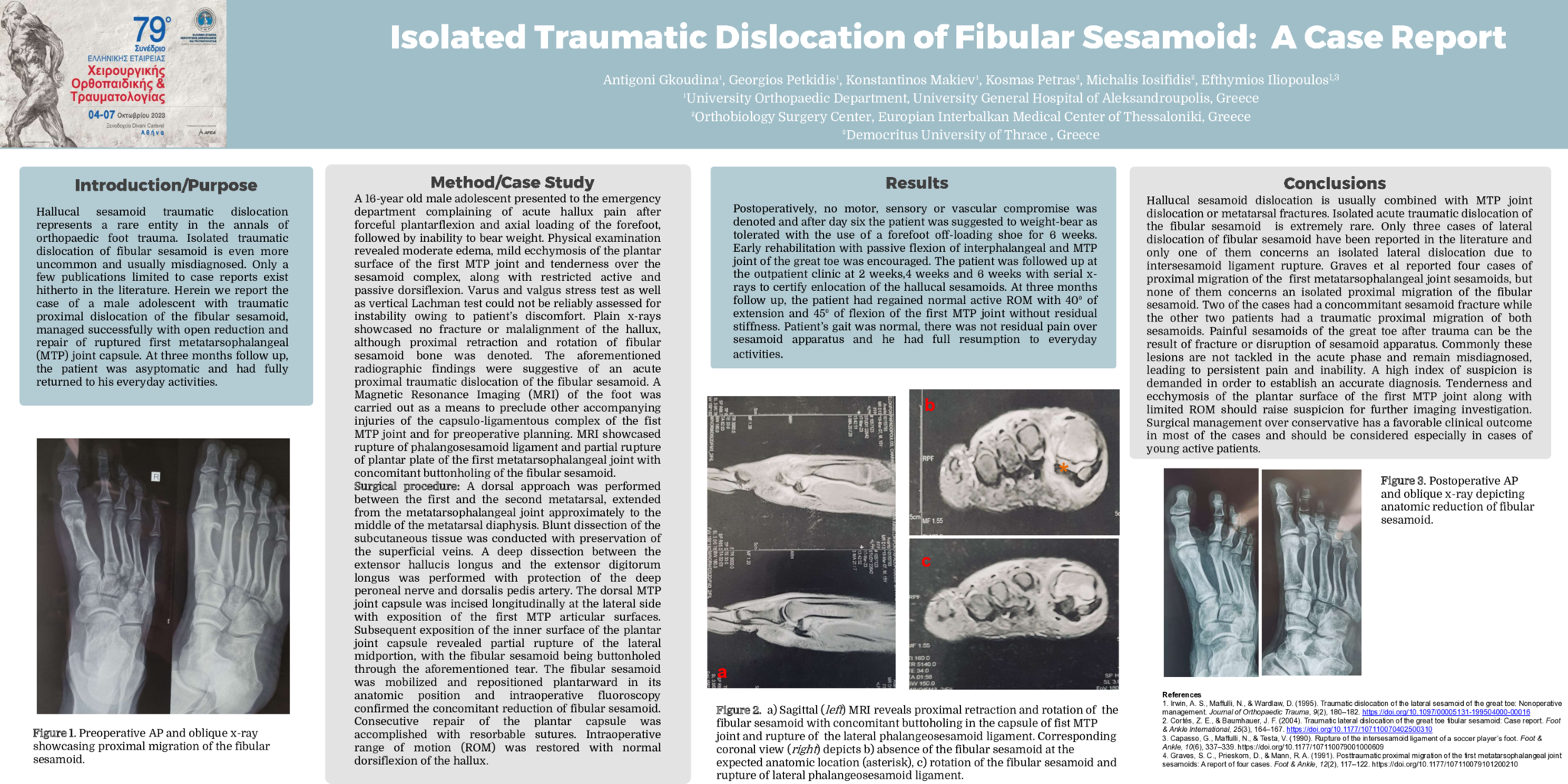
A 16-year old male adolescent presented to the emergency department complaining of acute hallux pain after forceful plantarflexion and axial loading of the forefoot, followed by inability to bear weight. Physical examination revealed moderate edema, mild ecchymosis of the plantar surface of the first MTP joint and tenderness over the sesamoid complex, along with restricted active and passive dorsiflexion. Varus and valgus stress test as well as vertical Lachman test could not be reliably assessed for instability owing to patient’s discomfort. Plain x-rays showcased no fracture or malalignment of the hallux, although proximal retraction and rotation of fibular sesamoid bone was denoted. The aforementioned radiographic findings were suggestive of an acute proximal traumatic dislocation of the fibular sesamoid. A Magnetic Resonance Imaging (MRI) of the foot was carried out as a means to preclude other accompanying injuries of the capsulo-ligamentous complex of the fist MTP joint and for preoperative planning. MRI showcased rupture of phalangosesamoid ligament and partial rupture of plantar plate of the first metatarsophalangeal joint with concomitant buttonholing of the fibular sesamoid.
Surgical procedure: A dorsal approach was performed between the first and the second metatarsal, extended from the metatarsophalangeal joint approximately to the middle of the metatarsal diaphysis. Blunt dissection of the subcutaneous tissue was conducted with preservation of the superficial veins. A deep dissection between the extensor hallucis longus and the extensor digitorum longus was performed with protection of the deep peroneal nerve and dorsalis pedis artery. The dorsal MTP joint capsule was incised longitudinally at the lateral side with exposition of the first MTP articular surfaces. Subsequent exposition of the inner surface of the plantar joint capsule revealed partial rupture of the lateral midportion, with the fibular sesamoid being buttonholed through the aforementioned tear. The fibular sesamoid was mobilized and repositioned plantarward in its anatomic position and intraoperative fluoroscopy confirmed the concomitant reduction of fibular sesamoid. Consecutive repair of the plantar capsule was accomplished with resorbable sutures. Intraoperative range of motion (ROM) was restored with normal dorsiflexion of the hallux.
Results
Postoperatively, no motor, sensory or vascular compromise was denoted and after day six the patient was suggested to weight-bear as tolerated with the use of a forefoot off-loading shoe for 6 weeks. Early rehabilitation with passive flexion of interphalangeal and MTP joint of the great toe was encouraged. The patient was followed up at the outpatient clinic at 2 weeks,4 weeks and 6 weeks with serial x-rays to certify enlocation of the hallucal sesamoids. At three months follow up, the patient had regained normal active ROM with 40⁰ of extension and 45⁰ of flexion of the first MTP joint without residual stiffness. Patient’s gait was normal, there was not residual pain over sesamoid apparatus and he had full resumption to everyday activities.
Conclusions
Hallucal sesamoid dislocation is usually combined with MTP joint dislocation or metatarsal fractures. Isolated acute traumatic dislocation of the fibular sesamoid is extremely rare. Only three cases of lateral dislocation of fibular sesamoid have been reported in the literature and only one of them concerns an isolated lateral dislocation due to intersesamoid ligament rupture. Graves et al reported four cases of proximal migration of the first metatarsophalangeal joint sesamoids, but none of them concerns an isolated proximal migration of the fibular sesamoid. Two of the cases had a concommitant sesamoid fracture while the other two patients had a traumatic proximal migration of both sesamoids. Painful sesamoids of the great toe after trauma can be the result of fracture or disruption of sesamoid apparatus. Commonly these lesions are not tackled in the acute phase and remain misdiagnosed, leading to persistent pain and inability. A high index of suspicion is demanded in order to establish an accurate diagnosis. Tenderness and ecchymosis of the plantar surface of the first MTP joint along with limited ROM should raise suspicion for further imaging investigation. Surgical management over conservative has a favorable clinical outcome in most of the cases and should be considered especially in cases of young active patients.
- 3 προβολές