Introduction: Periprosthetic fractures around total knee replacements (TKRs) are rare but challenging complications, ranging from 0.4% to 1.7%. Aim of the study: To describe the management of a Type 3 periprosthetic tibial fracture in an 87-year-old woman with TKR and to highlight the intraoperative challenges.
Materials & Methods:
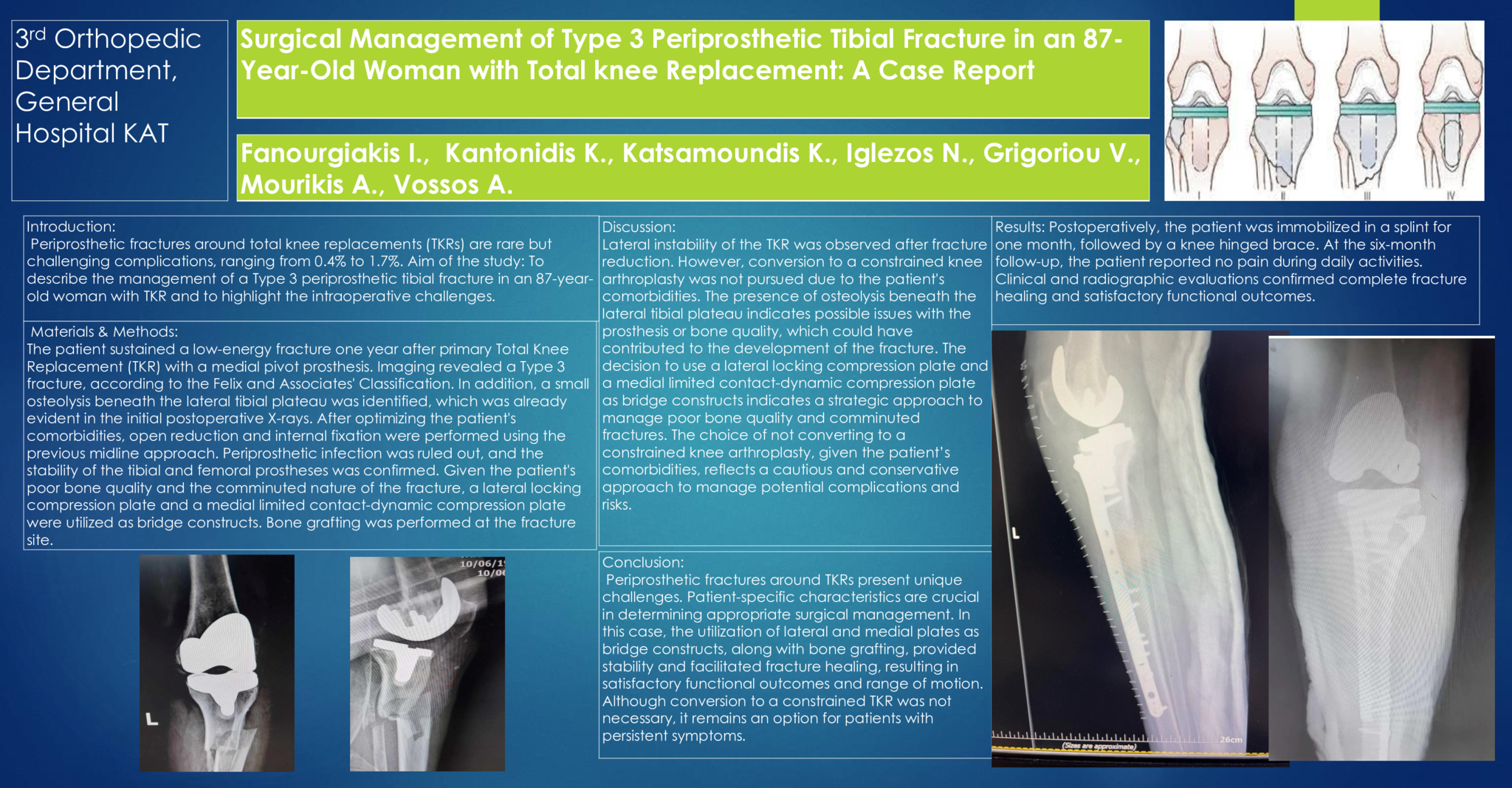
The patient sustained a low-energy fracture one year after primary Total Knee Replacement (TKR) with a medial pivot prosthesis. Imaging revealed a Type 3 fracture, according to the Felix and Associates' Classification. In addition, a small osteolysis beneath the lateral tibial plateau was identified, which was already evident in the initial postoperative X-rays. After optimizing the patient's comorbidities, open reduction and internal fixation were performed using the previous midline approach. Periprosthetic infection was ruled out, and the stability of the tibial and femoral prostheses was confirmed. Given the patient's poor bone quality and the comminuted nature of the fracture, a lateral locking compression plate and a medial limited contact-dynamic compression plate were utilized as bridge constructs. Bone grafting was performed at the fracture site.
Discussion:
Lateral instability of the TKR was observed after fracture reduction. However, conversion to a constrained knee arthroplasty was not pursued due to the patient's comorbidities. The presence of osteolysis beneath the lateral tibial plateau indicates possible issues with the prosthesis or bone quality, which could have contributed to the development of the fracture. The decision to use a lateral locking compression plate and a medial limited contact-dynamic compression plate as bridge constructs indicates a strategic approach to manage poor bone quality and comminuted fractures. The choice of not converting to a constrained knee arthroplasty, given the patient’s comorbidities, reflects a cautious and conservative approach to manage potential complications and risks.
Results: Postoperatively, the patient was immobilized in a splint for one month, followed by a knee hinged brace. At the six-month follow-up, the patient reported no pain during daily activities. Clinical and radiographic evaluations confirmed complete fracture healing and satisfactory functional outcomes
Conclusion: Periprosthetic fractures around TKRs present unique challenges. Patient-specific characteristics are crucial in determining appropriate surgical management. In this case, the utilization of lateral and medial plates as bridge constructs, along with bone grafting, provided stability and facilitated fracture healing, resulting in satisfactory functional outcomes and range of motion. Although conversion to a constrained TKR was not necessary, it remains an option for patients with persistent symptoms.
- 7 προβολές