INTRODUCTION
Ralstonia spp. are non-fermenting aerobic gram-negative rods, found in moist environments such as water, soil and plants. Ralstonia Mannitolilytica is one of the three members of the Ralstonia genus (R. Mannitolilytica, R. Pickettii and R. Insidiosa) that have been lately recognized for their role as human pathogens. Bone infections by the Ralstonia genus are very rare and only a few cases have been reported.
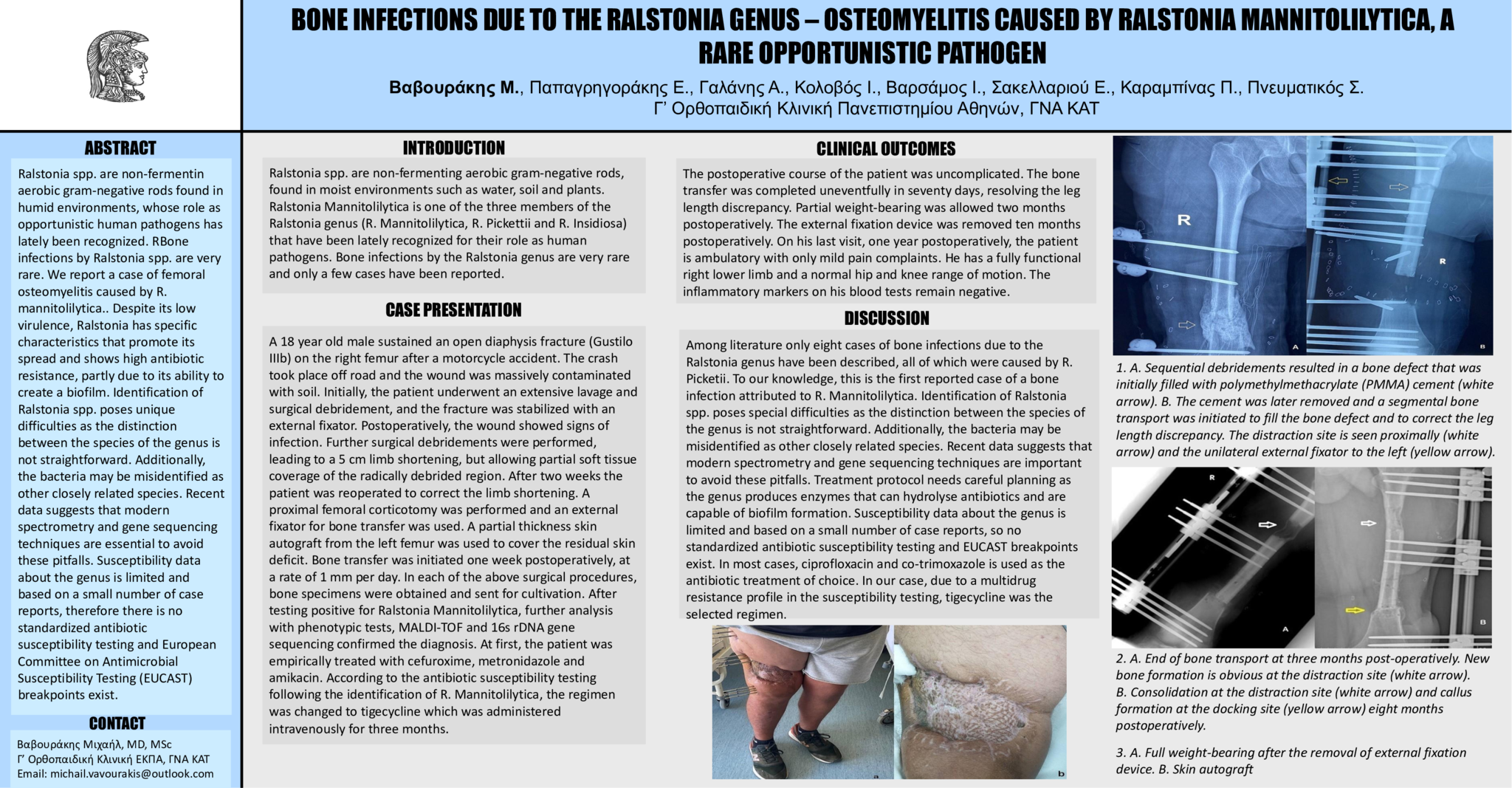
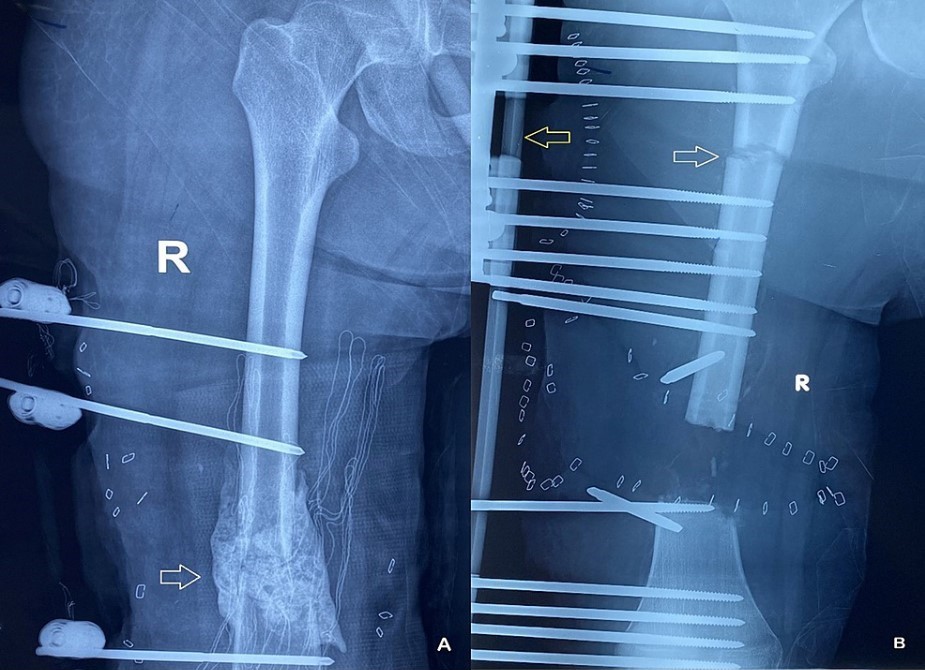
A 18 year old male sustained an open diaphysis fracture (Gustilo IIIb) on the right femur after a motorcycle accident. The crash took place off road and the wound was massively contaminated with soil. Initially, the patient underwent an extensive lavage and surgical debridement, and the fracture was stabilized with an external fixator. Postoperatively, the wound showed signs of infection. Further surgical debridements were performed, leading to a 5 cm limb shortening, but allowing partial soft tissue coverage of the radically debrided region. After two weeks the patient was reoperated to correct the limb shortening. A proximal femoral corticotomy was performed and an external fixator for bone transfer was used. A partial thickness skin autograft from the left femur was used to cover the residual skin deficit. Bone transfer was initiated one week postoperatively, at a rate of 1 mm per day. In each of the above surgical procedures, bone specimens were obtained and sent for cultivation. After testing positive for Ralstonia Mannitolilytica, further analysis with phenotypic tests, MALDI-TOF and 16s rDNA gene sequencing confirmed the diagnosis. At first, the patient was empirically treated with cefuroxime, metronidazole and amikacin. According to the antibiotic susceptibility testing following the identification of R. Mannitolilytica, the regimen was changed to tigecycline which was administered intravenously for three months.
CLINICAL OUTCOMES
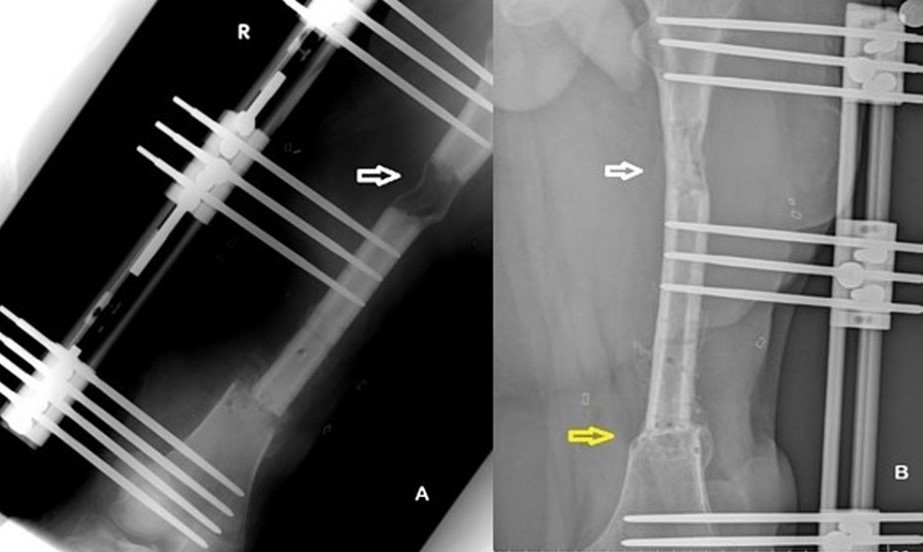
The postoperative course of the patient was uncomplicated. The bone transfer was completed uneventfully in seventy days, resolving the leg length discrepancy. Partial weight-bearing was allowed two months postoperatively. The external fixation device was removed ten months postoperatively. On his last visit, one year postoperatively, the patient is ambulatory with only mild pain complaints. He has a fully functional right lower limb and a normal hip and knee range of motion. The inflammatory markers on his blood tests remain negative.
DISCUSSION
Among literature only eight cases of bone infections due to the Ralstonia genus have been described, all of which were caused by R. Picketii. To our knowledge, this is the first reported case of a bone infection attributed to R. Mannitolilytica. Identification of Ralstonia spp. poses special difficulties as the distinction between the species of the genus is not straightforward. Additionally, the bacteria may be misidentified as other closely related species. Recent data suggests that modern spectrometry and gene sequencing techniques are important to avoid these pitfalls. Treatment protocol needs careful planning as the genus produces enzymes that can hydrolyse antibiotics and are capable of biofilm formation. Susceptibility data about the genus is limited and based on a small number of case reports, so no standardized antibiotic susceptibility testing and EUCAST breakpoints exist. In most cases, ciprofloxacin and co-trimoxazole is used as the antibiotic treatment of choice. In our case, due to a multidrug resistance profile in the susceptibility testing, tigecycline was the selected regimen.
B. Consolidation at the distraction site (white arrow) and callus formation at the docking site (yellow arrow) eight months postoperatively.

- 6 προβολές