Introduction
The hand is the most often traumatized part of a child body with phalangeal fractures to take the first place. Although most hand fractures in the pediatric population are stable and can be reduced and treated conservatively, some fractures like the phalangeal fractures needs special attention. Unstable proximal phalanx fractures can lead to malunion.
Finger overlap due to proximal phalange rotation malunion may cause pain, functional disability as well as unacceptable cosmetic appearance. This deformity can be treated by phalangeal or metacarpal rotational osteotomy. However postoperative complications mainly the contracture of the proximal interphalangeal joint remains as challenging issue.
Purpose
In this paper we review the literature, and present our case of a young boy with post-traumatic little finger overlap treated with rotational proximal phalanx osteotomy and double ray plate. We will try to discuss, comprehensively, the surgical techniques, complications and limitations of both osteotomies.
Materials and methods
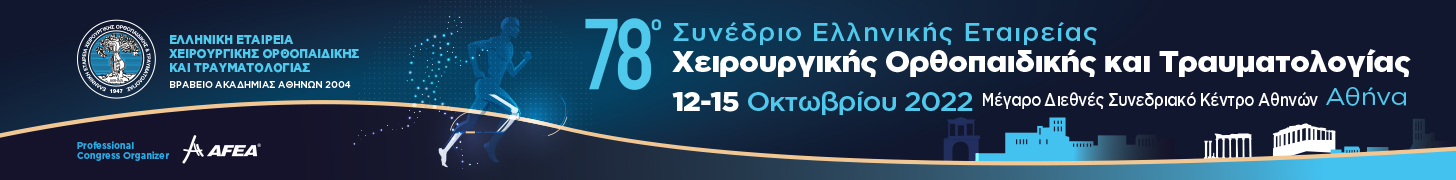
A 13-year-old, competitive swimmer, have been treated at the emergency clinic of our hospital for an oblique fracture of the proximal phalanx of his left little finger. An aluminum sling was used. Two weeks later, in the subacute phase, we noticed displacement of the fracture, and a close reduction attempt failed. Five weeks later, the phalange malunited in an obvious rotation with pain and contracture to the PIP joint. After two more weeks physiotherapy, we performed a rotation osteotomy of the proximal phalange, proximal to the fracture region, and stabilized it with double ray plate. Early range of movement was encouraged. We followed up the patient for 12 months.
We searched Google scholar for articles related to rotational malunion of long fingers related to proximal phalange fractures. We excluded articles of rotational malunions of the adult population, those due to metacarpal fractures and those of the thumb.
Results
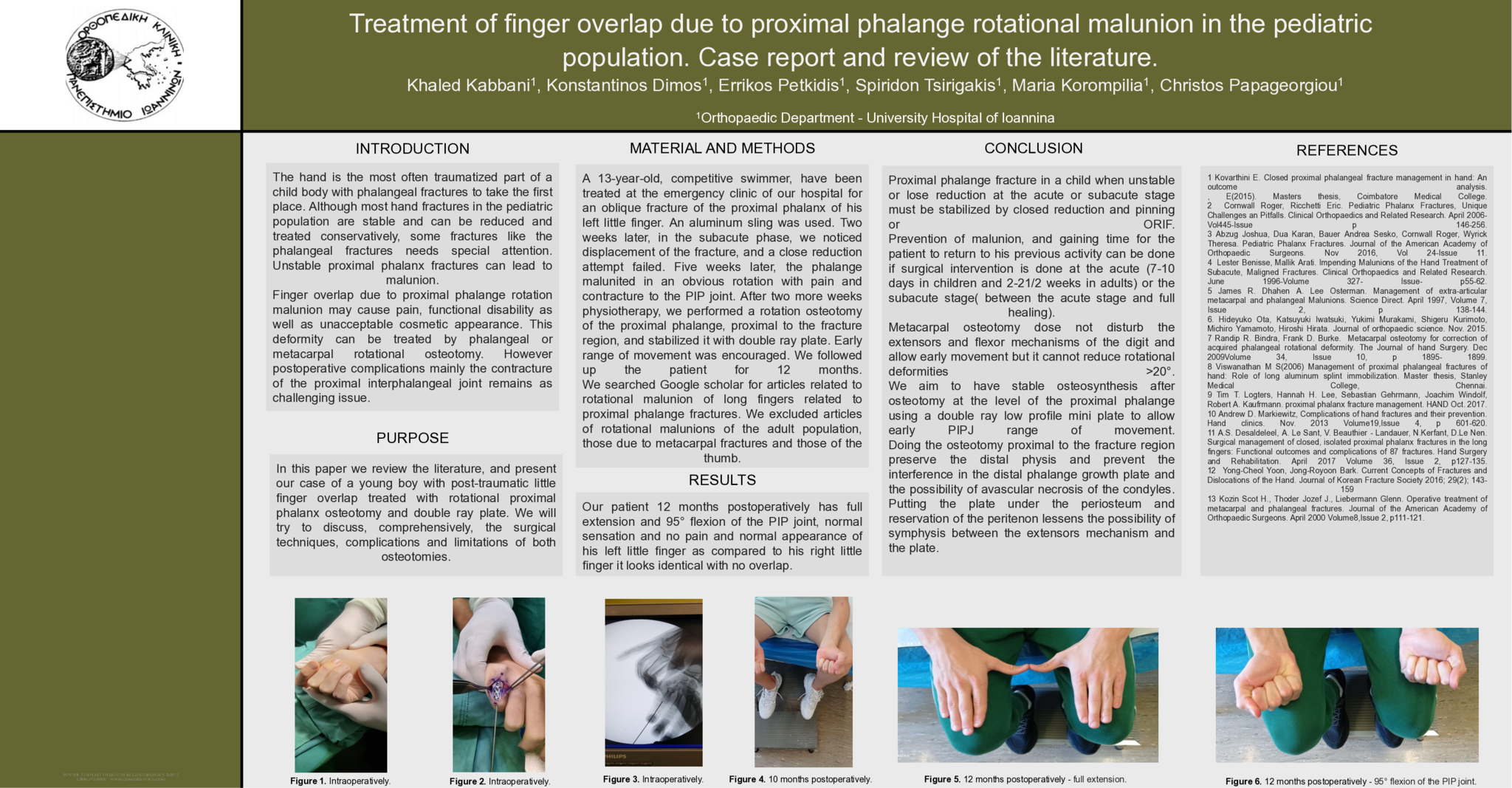
Our patient 12 months postoperatively has full extension and 95° flexion of the PIP joint, normal sensation and no pain and normal appearance of his left little finger as compared to his right little finger it looks identical with no overlap.
Conclusion
Proximal phalange fracture in a child when unstable or lose reduction at the acute or subacute stage must be stabilized by closed reduction and pinning or ORIF.
Prevention of malunion, and gaining time for the patient to return to his previous activity can be done if surgical intervention is done at the acute or the subacute stage.
Metacarpal osteotomy dose not disturb the extensors and flexor mechanisms of the digit and allow early movement but it cannot reduce rotational deformities >20°.
We aim to have stable osteosynthesis after osteotomy at the level of the proximal phalange using a double ray low profile mini plate to allow early PIPJ range of movement.
Doing the osteotomy proximal to the fracture region preserve the distal physis and prevent the interference in the distal phalange growth plate and the possibility of avascular necrosis of the condyles.
Putting the plate under the periosteum and reservation of the peritenon lessens the possibility of symphysis between the extensors mechanism and the plate.
References
1 Kovarthini E. Closed proximal phalangeal fracture management in hand: An outcome analysis.
, E(2015). Masters thesis, Coimbatore Medical College.
2 Cornwall Roger, Ricchetti Eric. Pediatric Phalanx Fractures, Unique Challenges an Pitfalls. Clinical Orthopaedics and Related Research. April 2006- Vol445-Issue p 146-256.
3 Abzug Joshua, Dua Karan, Bauer Andrea Sesko, Cornwall Roger, Wyrick Theresa. Pediatric Phalanx Fractures. Journal of the American Academy of Orthopaedic Surgeons. Nov 2016, Vol 24-Issue 11.
4 Lester Benisse, Mallik Arati. Impending Malunions of the Hand Treatment of Subacute, Maligned Fractures. Clinical Orthopaedics and Related Research. June 1996-Volume 327- Issue- p55-62.
5 James R. Dhahen A. Lee Osterman. Management of extra-articular metacarpal and phalangeal Malunions. Science Direct. April 1997, Volume 7, Issue 2, p 138-144.
6. Hideyuko Ota, Katsuyuki Iwatsuki, YukimiMurakami, Shigeru Kurimoto, Michiro Yamamoto, Hiroshi Hirata. Journal of orthopaedic science. Nov. 2015.
7 Randip R. Bindra, Frank D. Burke. Metacarpal osteotomy for correction of acquired phalangeal rotational deformity. The Journal of hand Surgery. Dec 2009Volume 34, Issue 10, p 1895- 1899.
8 Viswanathan M S(2006) Management of proximal phalangeal fractures of hand: Role of long aluminium splint immobilization. Master thesis, Stanley Medical College, Chennai.
9 Tim T. Logters, Hannah H. Lee, Sebastian Gehrmann, Joachim Windolf, Robert A. Kaufrmann. proximal phalanx fracture management. HAND Oct. 2017.
10 Andrew D. Markiewitz, Complications of hand fractures and their prevention. Hand clinics. Nov. 2013 Volume19,Issue 4, p 601-620.
11 A.S.Desaldeleel, A. Le Sant, V. Beauthier-Landauer, N.Kerfant, D.Le Nen. Surgical management of closed, isolated proximal phalanx fractures in the long fingers: Functional outcomes and complications of 87 fractures. Hand Surgery and Rehabilitation. April 2017 Volume 36, Issue 2, p127-135.
12 Yong-Cheol Yoon, Jong-Royoon Bark. Current Concepts of Fractures and Dislocations of the Hand. Journal of Korean Fracture Society 2016; 29(2); 143-159
13 Kozin Scot H., Thoder Jozef J., Liebermann Glenn. Operative treatment of metacarpal and phalangeal fractures. Journal of the American Academy of Orthopaedic Surgeons. April 2000 Volume8,Issue 2, p111-121.
- 18 προβολές