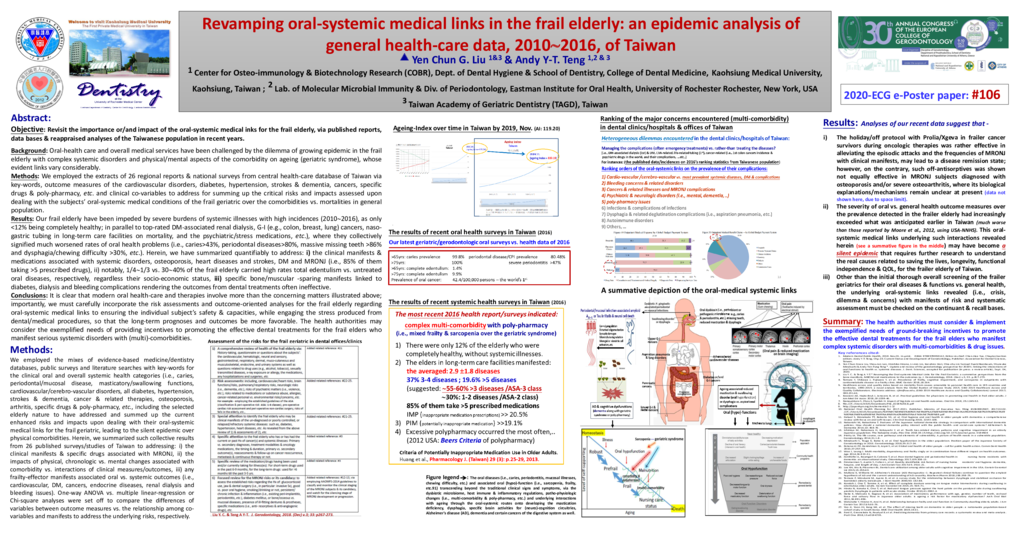
Background: Oral-health care and overall medical services have been challenged by the dilemma of growing epidemic in the frail elderly with complex systemic disorders and physical/mental aspects of the comorbidity on ageing (geriatric syndrome), whose evident links vary considerably. Methods: We employed the extracts of 26 regional reports & national surveys from central health-care database of Taiwan via key-words, outcome measures of the cardiovascular disorders, diabetes, hypertension, strokes & dementia, cancers, specific drugs & poly-pharmacy, etc. and clinical co-variables to address for summing up the critical risks and impacts assessed upon dealing with the subjects’ oral-systemic medical conditions of the frail geriatric over the comorbidities vs. mortalities in general population. Results: Our frail elderly have been impeded by severe burdens of systemic illnesses with high incidences (20102016), as only <12% being completely healthy; in parallel to top-rated DM-associated renal dialysis, G-I (e.g., colon, breast, lung) cancers, naso-gastric tubing in long-term care facilities on mortality, and the psychiatric/stress medications, etc.), where they collectively signified much worsened rates of oral health problems (i.e., caries>43%, periodontal diseases>80%, massive missing teeth >86% and dysphagia/chewing difficulty >30%, etc.). Herein, we have summarized quantifiably to address: i) the clinical manifests & medications associated with systemic disorders, osteoporosis, heart diseases and strokes, DM and MRONJ (i.e., 85% of them taking >5 prescribed drugs), ii) notably, 1/41/3 vs. 3040% of the frail elderly carried high rates total edentulism vs. untreated oral diseases, respectively, regardless their socio-economic status, iii) specific bone/muscular -sparing manifests linked to diabetes, dialysis and bleeding complications rendering the outcomes from dental treatments often ineffective. Conclusions: It is clear that modern oral health-care and therapies involve more than the concerning matters illustrated above; importantly, we must carefully incorporate the risk assessments and outcome-oriented analyses for the frail elderly regarding oro-systemic medical links to ensuring the individual subject’s safety & capacities, while engaging the stress produced from dental/medical procedures, so that the long-term prognoses and outcomes be more favorable. The health authorities may consider the exemplified needs of providing incentives to promoting the effective dental treatments for the frail elders who manifest serious systemic disorders with (multi)-comorbidities.
- 41 views